Underestimated and lethal! Such are the fungal invasive infections
By: Ximena Serrano Gil
Photos: Carolina Firacative, Ximena Serrano.
Health and Wellness
By: Ximena Serrano Gil
Photos: Carolina Firacative, Ximena Serrano.
Fungi. This word, by and large, conditions the popular imagination to picture representations of wild or edible mushrooms, nasty injuries on the skin, nails and hair or allergies, but beyond that, there are some that may cause the host’s death when invading the human body.
Yes, indeed, there are some fungal species that can trigger infections in the blood, brain, lungs, and other vital organs unless they are timely treated based on an adequate diagnosis. This has turned the invasive fungal diseases into underestimated and lethal enemies all over the world. Biologist and Medicine doctor Carolina Firacative, professor at the School of Medicine and Health Sciences of Universidad del Rosario and member of Studies in Translational Microbiology and Emerging Diseases Research Group (MICROS), in the same institution, has investigated the risk factors of those who develop such illnesses to recognize the impact of fungi-related infections in human health.
The scenario gets complex if we take into account that both in the environment and in every millimeter of our skin and mucosa, an endless number of microorganisms cohabit; many times, they are disregarded when it comes to assess a patient. The fact is that, in general, when it comes to infections, we tend to think about bacteria or viruses rather than fungi; therefore, the patient will not respond to the treatment because they are, biologically, quite different microorganisms.
Fungal diseases are an emerging issue worldwide. However, most of them are not taken into account when it comes to routine hospital attention as keeping a record of them at public health institutions is not mandatory.
That is why hundreds of thousands of people across the world, particularly those immunocompromised, suffering from cancer, HIV, transplants, and COVID-19, among other base conditions, are attacked each year by microorganisms like Candida albicans, Aspergillus fumigatus, and Cryptococus neoformans, the most common fungal species responsible for invasive pathologies in humans.
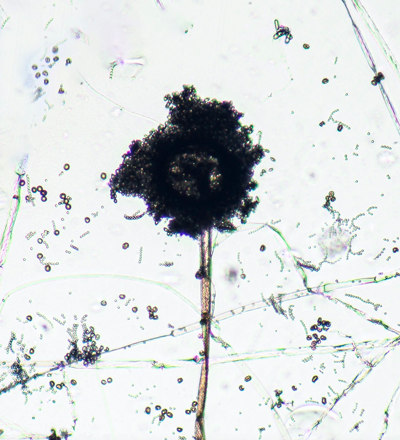
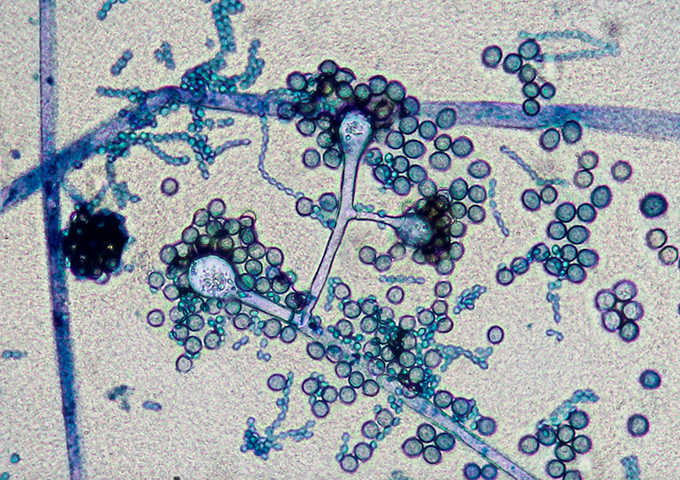
Photomicrograph of Aspergillus sp. conidiophores and conidia, one of the most common fungal pathogens causing invasive disease in humans. Lactophenol blue stain. 400X Magnification.

Carolina Firacative, professor at the Escuela de Medicina y Ciencias de la Salud(School of Medicine and Health Sciences) of the Universidad del Rosario, has researched other factors having an incidence in the complexity of these affections, such as the susceptibility of those pathogens to anti-fungal medicine.
Firacative indicates that many fungi are pathogens of key plants for agricultural activity, like tomato, potato, the banana tree, and a large number of flower crops that did not use to cause infections, but now they do. The tool to control them has been the application of fungicides. “These chemical products are similar, in their molecular composition and structure, to those taken by patients,” the expert warns. “If we take in such pathogens from an environment already exposed to agricultural drugs, that fungus may already be resistant to medicine.”
Such question is reinforced in the publication One Health: Fungal Pathogens of Humans, Animals and Plants, which explains that “the use of the same types of antifungal medicine in crop plants and in human beings generates an indirect selection pressure that increases the risk of developing strains resistant to the drugs used in antifungal therapy.”
These infections are never transmitted by intake; the problem arises when the infectious particles are cast over the crops, as the contact with the chemical products means that they will already present considerable levels of resistance; so, that drug will not be effective when the doctor treats the patient.
Fungal infections must also be considered
Although Carolina Firacative’s work contributes with findings and knowledge that feed the epidemiological global databases, the researcher highlights that beyond that effort, her role as teacher is to tell students that they should not think only of bacteria and virus as infection sources; they have to keep fungi in mind as well since in transplant patients, in serious medical condition, or in terminal stage, only the main condition is taken into account, and other possibilities are not considered, such as complications of their health derived from fungi, resulting in less recorded cases than what really occur.
“To me, the most important thing is to raise awareness among health care staff that their patients can be attacked by these infections, which must be timely identified, or otherwise the mortality rate increases,” the professor emphasizes.
In some way, medical advances also contribute to increase the number of people exposed to these risk factors, as in past years, maybe only 1 transplant per week was performed, and now, 20 are practiced. Other indicators that have gone up over time are the number of cancer patients and HIV positive cases (5,000 new cases annually in Colombia, according to the surveys by the Ministry of Health and Social Protection).
Based on all these reasons, the researcher insists on the importance of effective and truthful communication “among colleagues, infectologists, clinical laboratories, and nursing staff, as this best practice increases the speed of an adequate diagnosis, and therefore, it may help the patient to survive.”
What is a fungal disease?
Also known as mycosis, it is caused by a great variety of fungi which live both in the environment and in the microbiota (range of microorganisms living in the body).It becomes invasive when it brings about progressive infections in internal organs, which end up being lethal if not timely diagnosed and treated.
The infection may begin by inhaling infectious particles from the surroundings or by direct inoculation. However, fungi must meet four criteria to unleash an invasive disease in the human being:
- Being able to grow at or above mammalian body temperature.
- Getting to the internal tissue by penetrating or evading host barriers.
- Lysing tissues and absorbing their components.
- Having the ability to evade host immune defenses.
Prevention Measures
It is common to see prevention campaigns for viral or bacterial diseases, but not for those stemming from fungi. The following is a list of recommendations made by researcher Carolina Firacative, for a public health campaign:
- Do not take vegetable material to a hospital (flowers, fruit and not even plants in pots).
- Carry out a correct maintenance service to air-conditioning and heating systems.
- Control mold on walls, furniture, etc.
- Promote the frequent wash of hands among health care staff.
<
