In the “eye” of diabetes
By: Stefany Hernández
Photos: 123RF, Milagro Castro
Health and Wellness

By: Stefany Hernández
Photos: 123RF, Milagro Castro
This seems to be a priority in health. According to the World Health Organization’s (WHO) World Vision Report 2020, the eyes are the fourth most affected organ due to various diseases, including diabetes mellitus. However, this report only refers to the retina as the only tissue whose alteration can lead to blindness in diabetic patients. But why is the retina more relevant than the cornea in this chronic disease?
For Diana Patricia Amador, Professor of the School of Medicine and Health Sciences of Universidad del Rosario and PhD in Physiology, the answer lies in the relevance given to the cardiovascular and neurological impact to our body. The damage caused by the excess of glucose or “sugar” in the blood (also known as hyperglycemia) significantly affects the blood vessels and the nervous tissue.
Although the deterioration caused by diabetes is not known in detail, if we add other variables, it could lead to more corneal transplants to diabetic patients; a transplant is an extreme measure for the health care system.
These two systems are the mainly affected in other types of diseases, such as hypertension or kidney failure.
As Dr. Amador mentions, “guidelines for clinical practice worldwide do not stipulate that a medical check-up for a diabetic patient must include the evaluation of the endothelium and corneal pachymetry (medical exam that measures the thickness of the cornea).” She also states that the idea of a degeneration in the cornea as a secondary aspect came to light just a few years ago, but there is still a need of more research and prevention programs on the matter.
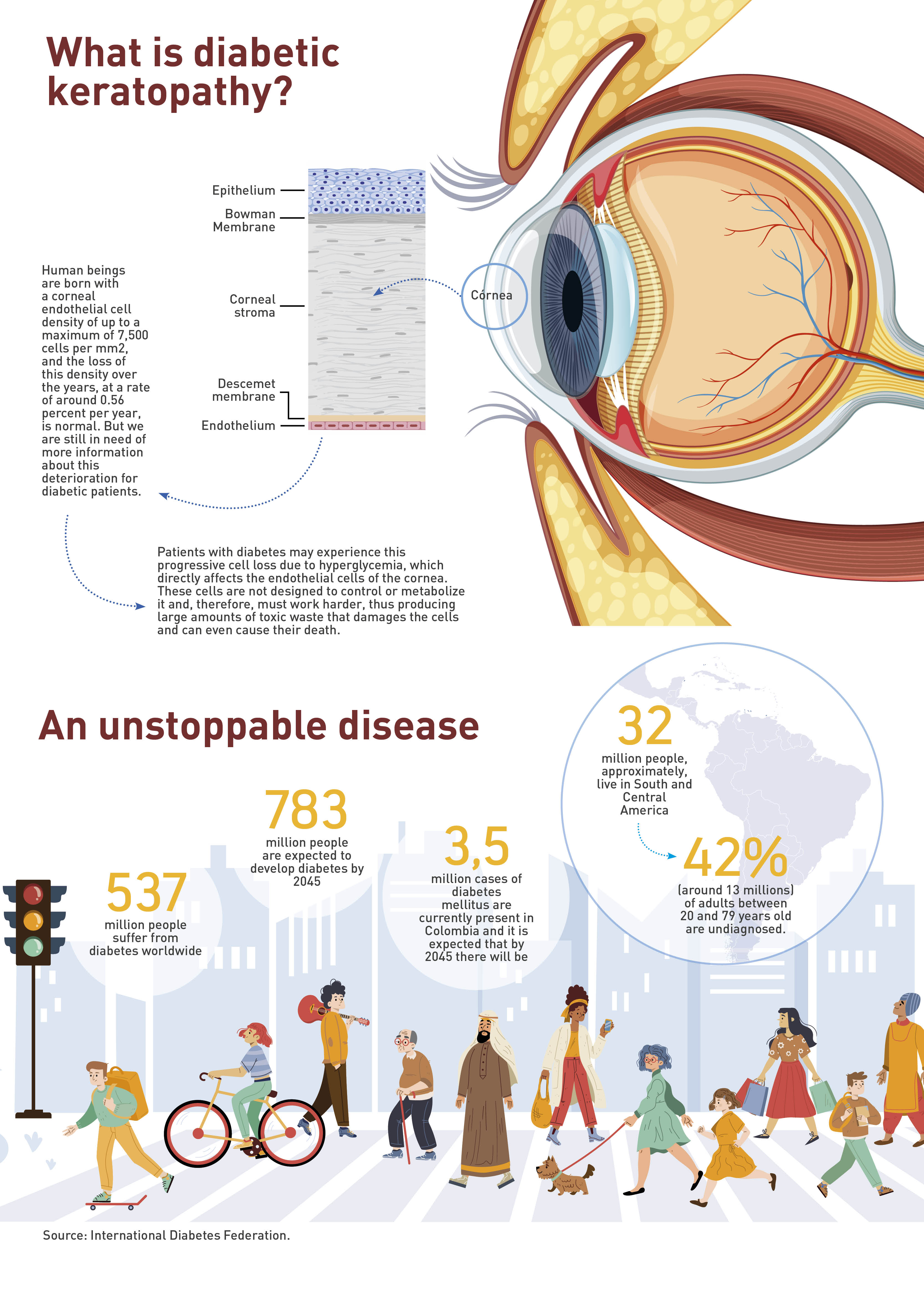
According to the International Diabetes Federation (IDF), by the year 2021, there were 537 million people with some type of diabetes in the world. It is estimated that there will be around 643 million by 2030. These figures are especially alarming because of the exponential increase in diagnoses. Developing countries are greatly affected by this disease, mainly due to the lack of regulation on food with high concentration of saturated fats and sugars, the lack of nutritional education, and access to certain healthy foods. In addition, there are high rates of sedentary lifestyles, alcohol consumption, and illicit drug use.
The problems caused by diabetes begin in the pancreas, where humans produce insulin, the hormone responsible for using the glucose from food as an energy source for all systems, organs, and tissues to work properly. When insulin is not produced, glucose accumulates in the blood, which, over time, leads to hyperglycemia and generates vascular and neurological damage, among others. Currently, the WHO recognizes three types of diabetes mellitus: gestational, Type 1, and Type 2
Pioneering research
Despite the fact that diabetes is considered one of the most lethal chronic diseases of the 21st century, scientific studies on the subject suggest that we still do not have enough information to prevent, treat, and improve the medical prognosis of patients suffering from it or of those at risk of developing it. However, in a recent study conducted by the Neuroscience Research Group (NeURos) of the School of Medicine and Health Sciences of Universidad del Rosario and published in Cornea, it was found that a stronger progressive deterioration in corneal endothelial cells appeared in patients with Type 1 diabetes compared with patients with Type 2 diabetes.
Dr. Amador explains that humans are born with a corneal endothelial cell density of up to a maximum of 7,500 cells per mm2, and the loss of this density over the years, at a rate of around 0.56 percent per year, is normal. But we are still in need of more information about this deterioration for diabetic patients.
The researchers began by focusing on cases of Type 1 diabetes because it is a disease that generally appears at an early age and has a more severe metabolic impact, therefore requiring more medical monitoring and follow-up.
But as the study progressed, they ran into a major hindrance: they found no records of Latin American or Colombian patients aged 0 to 5 years with Type 1 diabetes reporting corneal injury, which forced them to limit the study group to a population of children over 8 and young adults diagnosed with type 1 diabetes, who had a study or analysis of the corneal endothelium.
“I was surprised (for the case of Colombia) about the fact that we did not find any data on diabetic patients in terms of quantification of any of the corneal assessment criteria, since there are at least eight. Unfortunately, there was not a single document with these specifications, or with reports of pachymetry, endothelial count, or cellular variability... nothing,” says Dr. Diana Patricia Amador. For this reason, the study group collected data from 367 patients with Type 1 diabetes and 2,136 patients with Type 2 diabetes from human studies around the world, all of them with endothelial measurements and pachymetry studies.
The researchers’ conclusion after their analysis is that patients with Type 1 diabetes have greater cell loss in endothelium and corneal thickening than patients with Type 2 diabetes, regardless of age and gender. In other words, the cornea is damaged faster in the former group to the extent that there is a high probability that by the age of 30, patients with Type 1 diabetes will have the cornea of a 75-yearold or with such a level of opacity as to imply the need of a corneal transplant.
For the leader of the research group, “the idea is that not only the retina should be checked, but also the cornea, and that the degrees of damage should be identified as much as possible to prevent or delay of a corneal transplant.”

Diana Patricia Amador, researcher of the Escuela de Medicina y Ciencias de la Salud (School of Medicine and Health Sciences of Universidad del Rosario, explains that “guidelines for clinical practice worldwide do not stipulate that a medical check-up for a diabetic patient must include the evaluation of the endothelium and corneal pachymetry (medical exam that measures the thickness of the cornea)."
The heart of the matter lies in the fact that although the deterioration caused by diabetes is not known in detail, if we add other variables, it could lead to more corneal transplants to diabetic patients; a transplant is an extreme measure for the health care system.
Dr. Amador states that “It would be ideal to be more prepared, from the point of view of the healthcare staff, to face this impact that perhaps we have not yet identified in a very efficient way.”
In Colombia, the IDF recorded, for 2021, close to 3,200 cases of children between the ages of 0 and 19 with Type 1 diabetes mellitus; of these, there are no reports of keratopathy diagnosis or evolution, which is a cause for alarm since no long-term projections can be made to prevent harm to the visual health of diagnosed patients when they enter young or old age.
Currently, this study on diabetic keratopathy is under continuous and collaborative development by the NeURos Research Group together with other Colombian institutions, “and we hope that this is not the first and last to be conducted in the country on this subject,” concludes the expert.